We have with us a small excerpt of the import documents from Zauba and this sheds some light regarding the new Moto E (2016) which is currently code-named “Affinity”.The small snip doesn’t tell us much in specific regarding the phone except for its size and price.
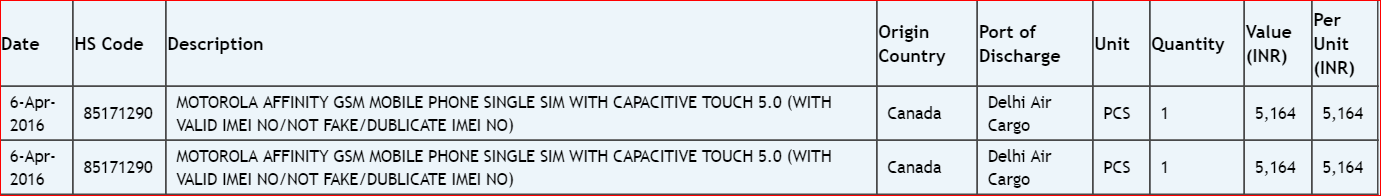
From the looks of Moto E 2016, it seems like the price of the device roughly amounts to 78$, or INR Rs.5,164 with a 5 inch display.The price is obviously not finalized but there wouldn’t be a dramatic change from the current 80$.Moreover the increase of the phone’s display from to 5 inches will be a welcome change for those looking into this device as all the current generations of the device have had only a 4.5 inch screen and to be honest 4.5inches is quit tiny considering how most of the people are now preferring bigger sized phones now.
Lenovo seems to be on a roll with the Moto device’s release with the Moto G model (2016) and now the Moto E (2016) as well and if the rumors and leaks are true then we’re probably set to see these 2 devices up for grabs by June , 2016. Until then lets wait and watch as the mystery regarding them unfolds .Keep checking the site for more updates regarding the device , cheers! Also, do tell us how excited are you and what do you think the next Moto E will bring this time, Comment down below!


