Can you imagine being so desperate for food that you would eat yourself to survive? Most people can’t but our cells do exactly this.
When cells are deprived of energy and nutrients from their external environment, they look internally, packaging up and consuming their own components to survive until an energy source becomes available. Once a food or nutrient source is available, cells are able to replace these components.
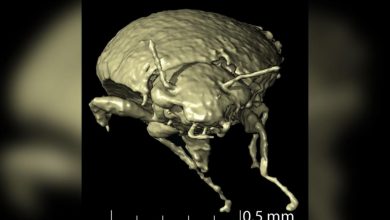
This cellular process is called autophagy, from “auto-” the Greek word for self and “phagein” meaning to eat. And cancer cells take advantage of this survival mechanism to evade some anti-cancer therapies.
Autophagy has remained largely unchanged across species throughout evolution occurring in organisms from yeast (simple cells) to eukaryotic (complex cells, like ours) systems in response to stressful conditions.
As we learn more about this process, we are garnering an understanding of how cancer cells survive therapy (from radiation to chemotherapy and novel targeted therapies) by digesting and recycling their own components to synthesise essential nutrients and provide energy.
Cancer hungry for energy
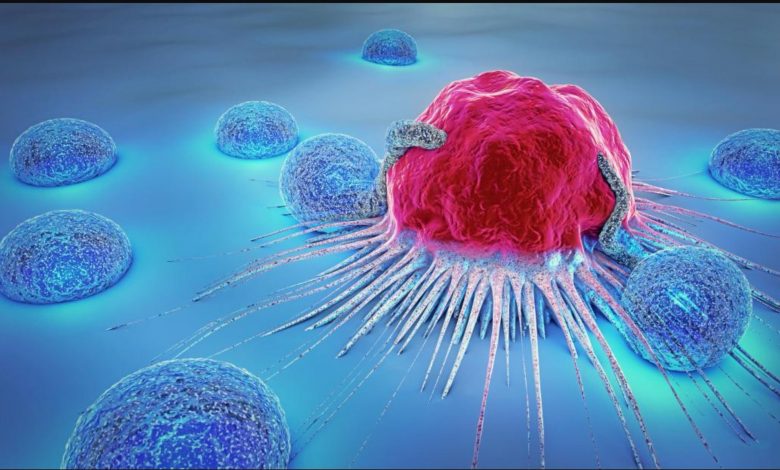
Cancer cells require a lot of energy to grow, make new cells and spread. They achieve this by harnessing survival processes used by normal, non-malignant cells.
Ordinarily, these survival processes are controlled by external factors, such as access to blood supply or growth signalling molecules from nearby cells. As these processes determine the life and death of non-malignant cells, they are highly regulated.
Importantly, in cancer cells these survival processes are independent of normal control mechanisms and therefore drive the uncontrolled growth and spread of the cancer.
In cancers such as chronic myeloid leukaemia where we know what drives the disease (a mutant gene, referred to as the oncogene, which tells the cells to multiply and progress), therapies target cancer cells while leaving non-malignant cells alone.
This targeted approach has also been utilised in other cancers in which the driver of disease is known, resulting in more personalised anti-cancer therapies with fewer side effects.
Such targeted treatments essentially starve cancer cells by blocking their survival processes. This causes their death and results in remission for most patients.
Cancer’s self-cannibalising survival
Resistance to therapy is an obstacle faced by both historic and current cancer therapies. One of the biggest challenges we now face in the development of new cancer treatments is persistent, low-level disease.
While some new treatments control cancer very well, cure is yet to be proven in many settings.
Work from our group recently demonstrated that when we use targeted therapy to attack cancer’s survival processes, such as signals to trigger cell growth, cancerous cells start to package up and consume their own contents.
Eating their own components allows them to generate the energy required to survive therapy. This results in persistent disease, or relapse.
Increasing evidence indicates that autophagy is a resistance mechanism used by several cancers, including, but not limited to, ovarian, pancreatic, brain, colon and breast cancers.
But if this is a survival mechanism on which several cancers converge, can we use our understanding of autophagy against cancer cells?
Eating itself to death
And the answer is yes, because of the vast and ever-increasing knowledge base about autophagy, we now know how to block it.
In a stroke of luck, we’ve even found a common drug used for other conditions that blocks autophagy. It does this by preventing the breakdown of cellular components.
When autophagy blockers are used in combination with targeted treatment in the leukaemia cells, the cells start to eat themselves, but are prevented from using what they consume for energy.
The cancer cells literally eat themselves to death.
Approaches targeting autophagy are now being taken into clinical trials in combination with anti-cancer therapy for leukaemia and other cancers.
“What we showed is that if this mechanism doesn’t work right, for example if autophagy is too high or if the target regulated by autophagy isn’t around, cancer cells may be able to rescue themselves from death caused by chemotherapies,” says Andrew Thorburn, PhD, deputy director of the CU Cancer Center.
A movie that accompanies the study online shows a cancer cell dying. In the first few frames, mitochondrial cell walls break down and the cell’s mitochondria can be seen releasing proteins in a process abbreviated as MOMP, which is considered a common marker of cell death. But then high autophagy allows the cell to encapsulate and “digest” these released proteins before MOMP can keep the cell well and truly dead. Later in the movie, the cancer cell recovers and goes on to divide.
“The implication here is that if you inhibit autophagy you’d make this less likely to happen, i.e. when you kill cancer cells they would stay dead,” Thorburn says.
Thorburn and colleagues including postdoctoral researcher Jacob Gump, PhD, show that autophagy depends on the target PUMA to regulate cell death. Specifically, when PUMA is absent, it doesn’t matter if autophagy is inhibited because without the communicating action of PUMA, cancer cells continue to survive.
The finding has important implications. First, it demonstrates a mechanism whereby autophagy controls cell death. And second, the study further reinforces the clinical potential of inhibiting autophagy to sensitize cancer cells to chemotherapy.
“Autophagy is complex and as yet not fully understood,” Thorburn says. “But now that we see a molecular mechanism whereby cell-fate can be determined by autophagy, we hope to discover patient populations that could benefit from drugs that inhibit this action.”
Cancer is responsible for over eight million deaths worldwide every year (out of 46 million diagnoses). By investigating how cancer cells avoid being killed when patients are on therapy, we can more effectively treat cancers by “eating” cancer at its own game. And that’s exactly what we’re doing.