NASA’s James Webb Space Telescope has captured a detailed image of the Sagittarius C region near the Milky Way’s core, revealing a dense star-forming area with numerous protostars and infrared-dark clouds. This observation offers new perspectives on star formation and the dynamics of our galaxy’s center. (Artist’s concept, see Webb image below.)
The play of darkness and light in our galaxy’s crowded core is put on display like never before.
A bright field of gas sweeps around the edge of a dark, dense cloud where young stars are bursting out to take their place in the universe. They join an estimated 500,000 other stars in the scene, of various ages, sizes, and colors. It’s the hub of our Milky Way galaxy, a city center at rush hour, making our solar system’s calm corner a frontier outpost by comparison. Discover the new features – and mysteries – NASA’s James Webb Space Telescope has revealed with its unprecedented infrared-light view of the chaotic region, and what it means for astronomy.

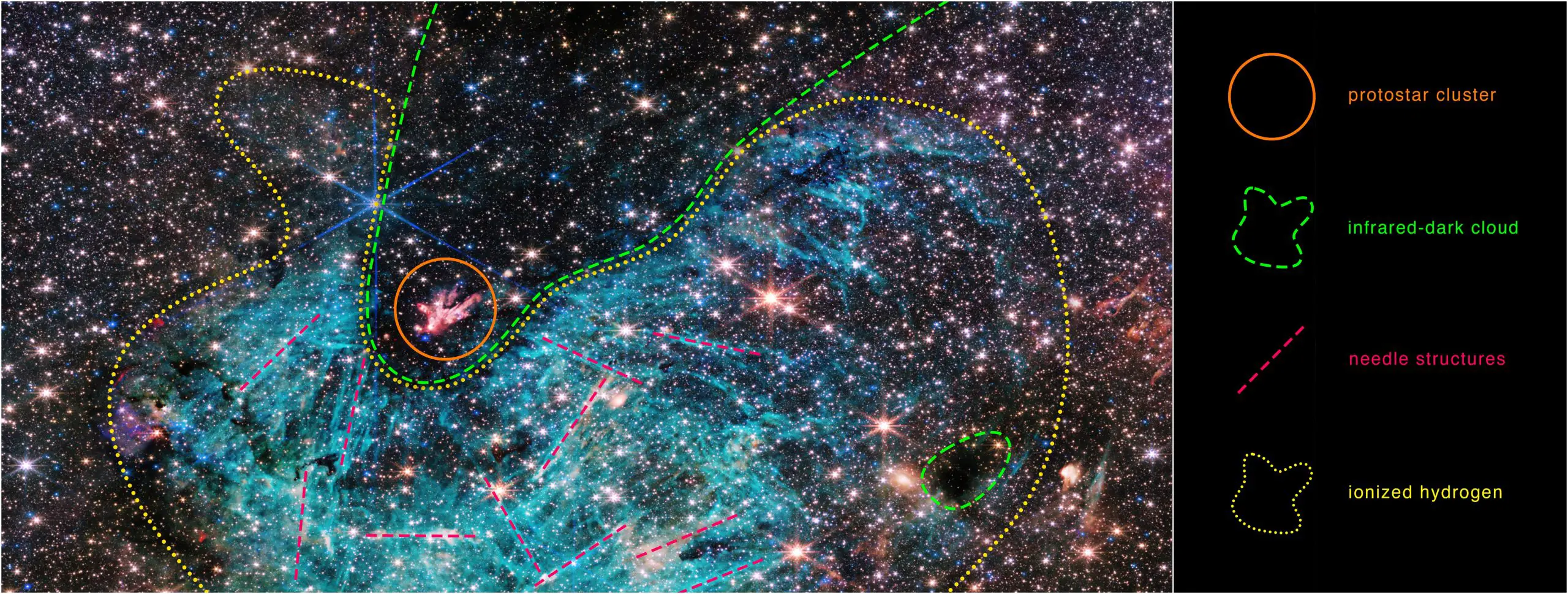
The full view of the James Webb Space Telescope’s NIRCam (Near-Infrared Camera) instrument reveals a 50 light-years-wide portion of the Milky Way’s dense center. An estimated 500,000 stars shine in this image of the Sagittarius C (Sgr C) region, along with some as-yet-unidentified features.
A vast region of ionized hydrogen, shown in cyan, wraps around an infrared-dark cloud, which is so dense that it blocks the light from distant stars behind it. Intriguing needle-like structures in the ionized hydrogen emission lack any uniform orientation. Researchers note the surprising extent of the ionized region, covering about 25 light-years.
Credit: NASA, ESA, CSA, STScI, Samuel Crowe (UVA)
Webb Space Telescope Reveals New Features in Heart of Milky Way
The latest image from NASA’s James Webb Space Telescope shows a portion of the dense center of our galaxy in unprecedented detail, including never-before-seen features astronomers have yet to explain. The star-forming region, named Sagittarius C (Sgr C), is about 300 light-years from the Milky Way’s central supermassive black hole, Sagittarius A*.
Unprecedented Detail
“There’s never been any infrared data on this region with the level of resolution and sensitivity we get with Webb, so we are seeing lots of features here for the first time,” said the observation team’s principal investigator Samuel Crowe, an undergraduate student at the University of Virginia in Charlottesville. “Webb reveals an incredible amount of detail, allowing us to study star formation in this sort of environment in a way that wasn’t possible previously.”
“The galactic center is the most extreme environment in our Milky Way galaxy, where current theories of star formation can be put to their most rigorous test,” added professor Jonathan Tan, one of Crowe’s advisors at the University of Virginia.
Protostars and Infrared-Dark Clouds
Amid the estimated 500,000 stars in the image is a cluster of protostars – stars that are still forming and gaining mass – producing outflows that glow like a bonfire in the midst of an infrared-dark cloud. At the heart of this young cluster is a previously known, massive protostar over 30 times the mass of our Sun. The cloud the protostars are emerging from is so dense that the light from stars behind it cannot reach Webb, making it appear less crowded when in fact it is one of the most densely packed areas of the image. Smaller infrared-dark clouds dot the image, looking like holes in the starfield. That’s where future stars are forming.
New Discoveries With NIRCam
Webb’s NIRCam (Near-Infrared Camera) instrument also captured large-scale emission from ionized hydrogen surrounding the lower side of the dark cloud, shown cyan-colored in the image. Typically, Crowe says, this is the result of energetic photons being emitted by young massive stars, but the vast extent of the region shown by Webb is something of a surprise that bears further investigation. Another feature of the region that Crowe plans to examine further is the needle-like structures in the ionized hydrogen, which appear oriented chaotically in many directions.

The north and east compass arrows show the orientation of the image on the sky. Note that the relationship between north and east on the sky (as seen from below) is flipped relative to direction arrows on a map of the ground (as seen from above).
The scale bar is labeled in light-years, which is the distance that light travels in one Earth-year. (It takes 3 years for light to travel a distance equal to the length of the scale bar.) One light-year is equal to about 5.88 trillion miles or 9.46 trillion kilometers. The field of view shown in this image is approximately 50 light-years long.
This image shows invisible near-infrared wavelengths of light that have been translated into visible-light colors. The color key shows which NIRCam filters were used when collecting the light. The color of each filter name is the visible light color used to represent the infrared light that passes through that filter.
Credit: NASA, ESA, CSA, STScI, Samuel Crowe (UVA)
Investigating the Galactic Center
“The galactic center is a crowded, tumultuous place. There are turbulent, magnetized gas clouds that are forming stars, which then impact the surrounding gas with their outflowing winds, jets, and radiation,” said Rubén Fedriani, a co-investigator of the project at the Instituto Astrofísica de Andalucía in Spain. “Webb has provided us with a ton of data on this extreme environment, and we are just starting to dig into it.”
Galactic Center Studies
Around 25,000 light-years from Earth, the galactic center is close enough to study individual stars with the Webb telescope, allowing astronomers to gather unprecedented information on how stars form, and how this process may depend on the cosmic environment, especially compared to other regions of the galaxy. For example, are more massive stars formed in the center of the Milky Way, as opposed to the edges of its spiral arms?
“The image from Webb is stunning, and the science we will get from it is even better,” Crowe said. “Massive stars are factories that produce heavy elements in their nuclear cores, so understanding them better is like learning the origin story of much of the universe.”
About the James Webb Space Telescope
The James Webb Space Telescope is the world’s premier space science observatory. It is leading investigations in our solar system, exploring distant worlds around other stars, and probing the mysterious structures and origins of our universe. Webb is an international program led by NASA, in collaboration with the European Space Agency (ESA) and the Canadian Space Agency.