Just few hours back, a new leak about another hyped Xiaomi device surfaced online. It’s still isn’t confirmed if it’s 100% true though, we believe the Redmi Pro 2 leak might be true as all previous leaks about the Xiaomi handsets were almost true! 🙂
The Smartphone is actually coming with some shit ass cool specs and we just can’t wait for some more new details! It was eventually spotted by the PlayfulDroid and they say- ” the device wold come with 6GB of RAM and 128GB of storage on the high end version and a lower version with 4GB + 64GB storage. Both storage versions vary in their prices which is also listed sa 1599 yuan & 1799 yuan respectively. There is also a 12MP Sony IMX362 rear sensor listed and a large 4,500mAh battery.”

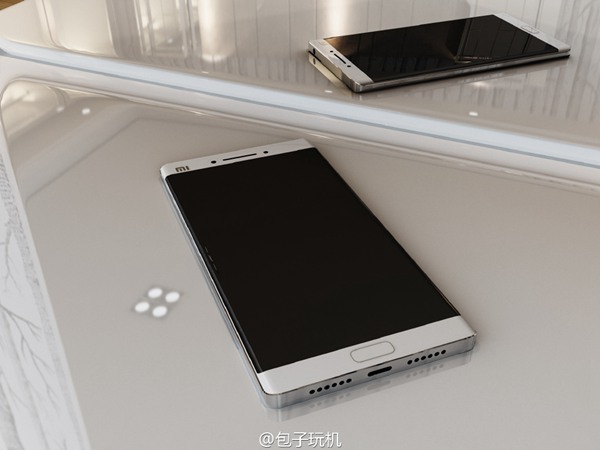
By looking at the leaked poster, the screen size of the device must be like 6″ or more. The design language looks pretty similar to other Xiaomi phones so Redmi Pro 2 won’t be that exciting in terms of design and looks.
We’ve have to see what the handset has to offer and also, we have to keep a look on other leaks too. We will notify you once we are up with another great leak! 😀 Cheers!
[Via: TrueTech | Source: PlayfulDroid]



