Motorola is working on a premium smartphone with flagship level specs, that will be released in the first quarter of 2021. The device is codenamed “nio” and the final name will be released later. Currently, there is no other phone or device with that specific refresh rate. Leaks related to the device have confirmed a current-generation Snapdragon 865 chip as well as midrange camera hardware from Motorola’s existing midrange devices. While the initial leaks confirmed a 90Hz refresh rate display on this phone, a recent spotting suggests the Motorola Nio will come with a faster 105Hz display.
Motorola is testing a default peak refresh rate of 105Hz for "nio". I've never seen a phone or display default to 105Hz, so it could just be something they're testing like how ASUS has a 160Hz mode on the ROG Phone 3. https://t.co/bUr8Jngek0
— Mishaal Rahman (@MishaalRahman) November 24, 2020
Mishaal Rahman of XDA Developers stated that the Nio will feature an unusual refresh rate of 105 Hz.
Before Asus launched their ROG Phone 3 gaming smartphone, the company was testing a 160Hz refresh rate mode on the device. However, the final device came with support for a 144Hz refresh rate while the 160Hz refresh rate could be enabled through a hidden code using the android platform tools. Rahmaan revealed that the Lenovo-owned brand is testing a default peak refresh rate of 105Hz for the Motorola Nio. He has speculated that the company could be simply testing a higher refresh rate as ASUS did on the ROG Phone 3. The final handset may come equipped with a 90Hz refresh rate. We believe that the 105Hz refresh rate could be an overclock of the phone’s existing refresh rate of 90Hz.

Motorola Nio specifications (Rumored)
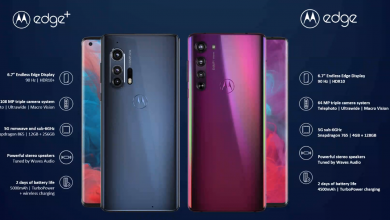
A previous leak already suggests that Motorola will go high on the cameras with the Nio. There wil be a 64-megapixel main camera along with a 16-megapixel ultra-wide camera and a 2-megapixel macro camera. For selfies, there will be a 16-megapixel wide camera at the front along with an 8-megapixel ultra-wide camera.
The Motorola Nio’s display produces a Full HD+ resolution of 1080 x 2520 pixels. Some leaks have confirmed a 6.7 inch display size and it is revealed that it has a punch-hole cutout for its dual front-facing cameras. The dual selfie camera system of the phone has a main camera of 16-megapixel and an 8-megapixel second lens. There is a triple camera system on the back of the Motorola Nio. The main camera is a 64-megapixel primary shooter, a 16-megapixel ultrawide lens, and a 2-megapixel depth assist lens. The smartphone is loaded with Android 11 OS and it is backed by a 5,000mAh battery.
As we stated earlier, the Snapdragon 865 completes the package, and it is expected to arrive in a 2 RAM/storage variants. 8/128 and 12/256. The handset model is said to be XT2125. Nothing is known as yet about the colours, but we should know that when the handset launches.